By Ethan Covey
People who identify as Hispanic, Black, Asian or other racial minority groups are far less likely to receive COVID-19 therapies, particularly monoclonal antibody (mAb) treatment, than white patients, in a new study.

The findings are the latest example of inequitable medical treatment of certain groups that has resulted in the COVID-19 pandemic having an outsized effect on nonwhite individuals, according to the epidemiologists (MMWR Morb Mortal Wkly Rep 2022;71:96-102).
“Equitable receipt of COVID-19 treatments by race and ethnicity, along with other prevention practices, plus management of underlying conditions that put a person at high risk, are essential to reduce inequities in severe COVID-19?associated illness and death,” said lead author Jennifer L. Wiltz, MD, the deputy medical director of the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
The study reviewed data from March 2020 through August 2021, obtained from 41 U.S. healthcare systems included in the National Patient-Centered Clinical Research Network (PCORnet).
Among patients who tested positive for COVID-19, Hispanic patients received mAb treatment less often than non-Hispanic patients; and Black, Asian and other minority patients received mAb treatment less often than whites. The mean prevalence of monthly mAb use among all patients with positive SARS-CoV-2 test results who were white, Black, Asian or another race was 4.0%, 2.8%, 2.2% and 2.2%, respectively. Rates among patients of Hispanic and non-Hispanic ethnicity were 1.8% and 4%, respectively.
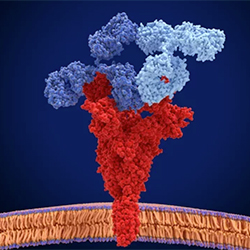
Delivery of mAbs can be complex. The therapy must be administered by IV infusion or subcutaneous injection by a healthcare provider, typically in outpatient settings, soon after receipt of a positive test result and within 10 days of symptom onset. Such factors, the epidemiologists noted, may combine with existing systemic factors like limited access to testing and care, inadequate insurance coverage and transportation challenges.
“The significance of the observed racial and ethnic disparities in mAb treatment is amplified by the fact that racial and ethnic minority groups are at increased risk for COVID-19 hospitalization and death,” Dr. Wiltz said. “As a result of longstanding systemic health and social inequities, racial and ethnic minority populations have higher rates of pre-existing conditions that place them at increased risk for severe COVID-19?associated outcomes.”
Disparities were also found in the inpatient administration of two COVID-19 therapies, the steroid dexamethasone and antiviral drug remdesivir, but they were smaller than those in mAb use. The study’s epidemiologists noted that this may be due, at least in part, to ease of medication access in hospitals.
The biggest inequalities were “in medication receipt in the outpatient setting,” Dr. Wiltz said.
As the pandemic changes and other treatments become available, future study will be key to illuminate how these disparities change. Treatments will include medications such as the oral antiviral agents nirmatrelvir tablets and ritonavir tablets (Paxlovid, Pfizer), molnupiravir (Merck) and sotrovimab (GSK), which is currently the only mAb effective against the omicron variant of SARS-CoV-2.
Until then, Dr. Wiltz noted that “understanding drivers and evidence-based action for equitable receipt of COVID-19 treatments by race and ethnicity is essential to reduce inequities in severe COVID-19?associated illness and death.
“Expanded research, resources, community partnerships and efforts are needed at multiple levels to make meaningful progress,” she added. “We hope this latest research inspires action across communities, clinical groups and sectors to address the gaps we’ve illuminated and bring us closer to equitable health for all.”