By Gina Shaw
The American Academy of Pediatrics (AAP) issued an evidence-based immunization schedule for routine immunizations for infants, children and adolescents against 18 diseases, in a break from the CDC’s newly reconstituted Advisory Committee on Immunization Practices (ACIP).

It’s the first major divergence between the two organizations’ vaccine recommendations since the AAP first began aligning its guidance with the CDC’s in 1995 (Vaccine 2015;33[3]:405-414).
The AAP guidance, published Aug. 19, 2025, includes updated recommendations for respiratory syncytial virus (RSV), influenza and COVID-19 immunizations for pediatric populations. It strongly recommends COVID-19 vaccines for children between 6 months and 2 years of age. Shots also are advised for older children if parents choose to do so. The CDC’s guidance, by contrast, does not recommend COVID-19 vaccination for healthy children of any age, although it states that children may receive the vaccine in consultation with a physician.
“We extensively reviewed the most recently available data about COVID-19 risks in kids, as well as safety and effectiveness of available COVID-19 vaccines. It’s clear they are very safe for all populations. Among the reasons we decided to move to a risk-based recommendation for healthy older children is the fact that the hospitalization rate for young children and children with underlying medical conditions remains high, in line with rates for many of the other vaccine-preventable diseases for which we vaccinate,” said Sean O’Leary, MD, FAAP, the chair of the AAP Committee on Infectious Diseases, in a statement.
In addition to RSV, flu and COVID-19, the guidance included new recommendations on a pentavalent meningococcal vaccine from GSK, and a recommendation to start HPV vaccination at 9 to 12 years. The hepatitis B vaccine (recombinant) PreHevbrio (VBI Vaccines) has been discontinued and was removed from the schedule.
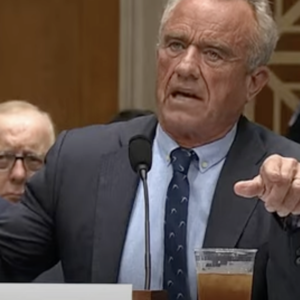
In May, Health and Human Services Secretary Robert F. Kennedy Jr. removed all 17 sitting members of the ACIP panel, which he claimed were biased, in a move that was decried by leading infectious disease and other health organizations, including the Infectious Diseases Society of America (IDSA), Society of Infectious Diseases Pharmacists, National Foundation for Infectious Diseases, Society for Healthcare Epidemiology of America, Pediatric Infectious Diseases Society, American Academy of Family Physicians, American Medical Association and AAP. He then replaced the panel with members who have criticized vaccines and spread vaccine misinformation.
“The AAP will continue to provide recommendations for immunizations that are rooted in science and are in the best interest of the health of infants, children and adolescents,” said AAP President Susan J. Kressly, MD, FAAP, in the statement. “Pediatricians know how important routine childhood immunizations are in keeping children, families and their communities healthy and thriving.”
Less than a week later, on Aug. 25, the American College of Obstetricians and Gynecologists (ACOG) issued its own guidelines regarding vaccination during pregnancy against COVID-19, influenza and RSV. ACOG recommends that patients receive an updated COVID-19 vaccine or booster at any point during pregnancy, when planning to become pregnant, in the postpartum period or when lactating, noting that data show that the COVID-19 vaccines are particularly effective at reducing morbidity from COVID-19 complications in pregnant patients and their infants.
ACOG also continues to strongly recommend that anyone who is or will be pregnant during influenza season receive an inactivated or recombinant influenza vaccine as soon as it is available, during any trimester of pregnancy, and that during RSV season, patients receive the bivalent RSVpreF vaccine (Abrysvo, Pfizer) in order to protect their infants after birth. “Patients should also understand that if they decline the maternal RSV vaccination, their infant needs a monoclonal antibody at birth,” the recommendations noted.
“It is well documented that respiratory conditions can cause poor outcomes during pregnancy, with pregnant women facing both severe illness and threats to the health of their pregnancy. Thanks to vaccines, severe outcomes from respiratory infections are largely preventable,” said Steven J. Fleischman, MD, MBA, FACOG, the president of ACOG, in a statement. “ACOG’s updated respiratory guidance documents repeat what we have long known: that vaccines continue to be the best tool available for pregnant patients to protect themselves and their infants from these viruses.”
In an X post, Mr. Kennedy called the AAP recommendations “corporate-friendly” and said physicians who follow them might not be covered under the National Childhood Injury Act. “AAP should also be candid with doctors and hospitals that recommendations that diverge from the CDC’s official list are not shielded from liability under the 1986 Vaccine Injury Act,” he wrote.
This is misleading, according to Dorit Reiss, PhD, a law professor at the University of California, San Francisco. In a Facebook post, Dr. Reiss said coverage under the National Childhood Vaccine Injury Act depends on whether the vaccine is listed by Congress as a covered vaccine in the Vaccine Injury Compensation Program (VICP), not on who recommends it. “If a vaccine is covered by VICP, liability protections apply to manufacturers and administrators: anyone claiming a vaccine harm from a childhood vaccine that is under VICP has to go through the program first. ACIP has not actually changed the current recommendations in ways that affect VICP,” she wrote.
She added that COVID-19 vaccines are not covered under VICP because Congress has not created an excise tax for COVID-19 vaccines; VICP funds are provided by an excise tax placed on that vaccine.
“There’s still a PREP [Public Readiness and Emergency Prepardness] Act declaration shielding manufacturers and administrators, and those vaccines fall under the separate program, CICP [the Countermeasures Injury Compensation Program],” she said.
For years, medical specialty societies such as the AAP, ACOG and IDSA have issued their own recommendations tailored to specific populations such as children, pregnant women and immunocompromised individuals. Until the new ACIP, those guidelines were based on the ACIP recommendations.
“What is different now is that previously, these organizations were able to rely on ACIP for their recommendations, and for a data resource upon which to make decisions about their own recommendations,” said Michael Osterholm, PhD, MPH, the Regents Professor, McKnight Presidential Endowed Chair in Public Health, and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota, in Minneapolis. “One of the biggest challenges we have now is that we have to question whether any of the information that comes out of HHS today can be trusted to be scientifically sound. We never have had to say that before in my 50 years in the business. This is a first and it’s a tragic first.”
Dr. Osterholm leads CIDRAP’s Vaccine Integrity Project, which collaborated with the AAP to assist in its development of the recommendations. Focused on developing and disseminating the evidence for immunization recommendations and clinical consideration, the Vaccine Integrity Project is “picking up where ACIP left off,” he said.
“We are developing the science base upon which medical societies and other organizations can make evidence-based vaccine recommendations. I think you will see multiple societies relying heavily on a combination of past ACIP data analyses up to early 2025, and then our analysis going forward. We have tried to provide that continuation. It’s unfortunate that we are in this position, but the most important message is that the scientific community is stepping up and working together to provide information and recommendations grounded in peer-reviewed science.”
In a public webinar on Aug. 19, 2025, the Vaccine Integrity Project presented data from its comprehensive evidence review on the safety and efficacy of the U.S. influenza, RSV and COVID-19 vaccines ahead of the upcoming respiratory virus season. The presentation focused on the COVID-19 and RSV vaccines in pregnant women, children and those with weakened immune systems.
For the review, 24 experts in infectious diseases and epidemiology screened some 16,000 abstracts and reviewed 1,406 full-text articles published over recent respiratory virus seasons, and selected 590 papers for detailed data extraction, including 50 randomized controlled trials.
“The new data do not indicate the emergence of a safety signal or a sudden drop in effectiveness of these immunizations,” Dr. Osterholm said during the webinar. “There is no scientific evidence to support the changes HHS made to COVID recommendations for pregnant women or for children.”
The review also failed to find any new evidence of safety signals related to myocarditis after COVID-19 vaccination, but it did detect a potential risk for preterm birth linked to the RSV vaccine for pregnant women.
“One new study supported the effectiveness of influenza vaccination in pregnancy to reduce medically attended infection and in pregnant women,” Dr. Osterholm said. “For all other studies reviewed, COVID, RSV and influenza vaccination resulted in similar or better outcomes compared to no vaccination. Of the close to 17,000 abstracts reviewed and nearly 600 papers extracted, autism was not raised as a significant adverse event.”
The Vaccine Integrity Project has emerged as “the place where the trusted scientists are going to land,” said Elizabeth Dodds Ashley, PharmD, a professor of medicine in the Division of Infectious Diseases and International Health at Duke University, in Durham, N.C. “It is multidisciplinary, inclusive and has a lot of seats at the table for all of the leading stakeholders,” she said. “It’s clear that they did a very thorough job reviewing the data they presented in the webinar and demonstrating why we do not support the changes that were made by HHS. They’ve really turned the ship very quickly and begun to fill the void left by HHS on vaccine recommendations.”
The next concern: ensuring that the recommended vaccines are fully covered by health insurance. The AAP said it has been in communication with payors to ensure that the recommended vaccines will be covered, and urged all insurers to cover all vaccines included in the schedule. “Recommendations are one thing; access to vaccines is another,” Dr. Dodds Ashley said. “Now that we have the scientists together saying what they need to say, in a format we can all access, we need all the payors to listen to that.”
The sources reported no relevant financial disclosures.