By IDSE News Staff
The number of reports about serious adverse events (AEs) among patients exposed to fentanyl, heroin and other illicit drugs contaminated with xylazine are increasing, according to the FDA, which issued a warning to healthcare providers.
Stimulants (e.g., methamphetamine and cocaine) also have been combined with xylazine. Xylazine-containing products may be sold under the street names tranq, tranq dope, sleep-cut, Philly dope and zombie drug. There have been reports of individuals combining xylazine with speedball (i.e., an opioid used with a stimulant) to offset unintended effects of the individual components of the mixture, according to the alert.
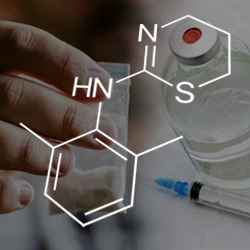
Xylazine is a nonopioid agent approved for use in veterinary medicine as a sedative and pain reliever. Structurally, xylazine is similar to clonidine, levamisole and tizanidine and may share some clinical effects. Like clonidine, xylazine acts as a central alpha-2 adrenergic receptor agonist in the brainstem, causing a rapid decrease in the release of norepinephrine and dopamine in the central nervous system (CNS). Xylazine also may bind to other CNS receptors.
Xylazine is not approved for use in humans and may result in serious and life-threatening AEs that appear to be similar to those associated with opioid use, making it difficult to distinguish opioid overdoses from xylazine exposure.
“However, we do not know if side effects from xylazine exposure can be reversed by naloxone,” the FDA said in the warning. “Since we do not know if reversal agents regularly used in veterinary medicine (e.g., yohimbine hydrochloride, tolazoline hydrochloride) are safe or effective in humans, they should not be used.”
To make matters worse, routine toxicology screening does not detect xylazine, and additional analytical techniques are required to detect xylazine when it might be involved in illicit drug overdoses, particularly when there are other signs or symptoms of xylazine exposure.
Healthcare professionals should continue to administer naloxone for opioid overdoses and consider xylazine exposure if patients are not responding to naloxone, or when there are signs or symptoms of xylazine exposure, such as severe, necrotic skin ulcerations.
Healthcare professionals should provide appropriate supportive measures to patients who do not respond to naloxone.
The FDA issued a letter to stakeholders providing clinical information about the risks for severe, necrotic skin ulcerations from repeated xylazine exposure, possible withdrawal symptoms and xylazine’s interference with successful treatment of opioid overdoses.
Repeated exposure to xylazine, by injection, has been associated with severe, necrotic skin ulcerations that are distinctly different from other soft tissue infections, such as cellulitis, abscesses often associated with injection drug use. These lesions may develop in areas of the body away from the site of injection.
It is not known at this time whether the xylazine used in these scenarios is illicitly produced or diverted from the animal drug supply. The FDA is continuing to investigate the source of xylazine in the illicit drug supply.
The FDA encourages healthcare professionals and patients to report AEs in humans associated with possible illicit xylazine exposure to the FDA’s MedWatch Adverse Event Reporting program. Complete and submit the report online at www.fda.gov/medwatch/report.htm; or download and complete the form, then submit it via fax at (800) FDA-0178.
—From FDA press materials

