By IDSE News Staff
The CDC issued a health advisory about a recently confirmed outbreak of Ebola disease in Uganda caused by the Sudan virus (species Orthoebolavirus sudanense), recommending travelers returning from Uganda monitor themselves for symptoms of Sudan virus disease (SVD) while in the outbreak area and for 21 days after leaving.
Travelers should also self-isolate and contact local health authorities or a clinician if they develop symptoms. (Early “dry” symptoms may include fever, aches, pains and fatigue, and later “wet” symptoms may include diarrhea, vomiting and unexplained bleeding.)
On Feb. 5, 2025, the CDC issued a Travel Health Notice Level 2, which recommended enhanced precautions for people traveling to Uganda. However, the CDC has not issued any interim recommendations to health departments for post-arrival risk assessment and management of travelers, including U.S.-based healthcare professionals, arriving from Uganda.
There are no suspected, probable or confirmed Ebola cases related to this outbreak in the United States, or outside of Uganda. However, as a precaution, the CDC shared best practices for public health departments, public health and clinical laboratories, and healthcare professionals in the United States, the agency said.
On Jan. 29, the Ministry of Health of Uganda officially declared an Ebola outbreak caused by the SVD in the nation’s capital, Kampala. This is the eighth Ebola outbreak in Uganda since 2000. The confirmed case was in a 32-year-old male nurse at the Mulago National Referral Hospital. The man initially developed high fever, chest pains, difficulty in breathing and bleeding from multiple body sites and sought treatment at multiple health facilities, including Mulago Referral Hospital, in Kampala; Saidina Abubakar Islamic Hospital, in Matugga in Wakiso District; and Mbale Regional Referral Hospital, in Mbale City. He also sought treatment from a traditional healer. The patient died on Jan. 29. Post-mortem samples were tested and confirmed positive for SVD at three national reference laboratories. The CDC is working closely with the Ministry of Health of Uganda to support the response to this outbreak.
While there are no direct flights from Uganda to the United States, travelers from or passing through affected areas in Uganda can enter the United States on flights connecting from other countries.
Healthcare providers should evaluate any patients suspected of having SVD. It is important for clinicians to obtain a detailed travel history from patients with suspected SVD, especially those who have been in affected areas of Uganda. Early consideration of SVD in the differential diagnosis is important for providing appropriate and prompt patient care, diagnostics, and to prevent the spread of infection.
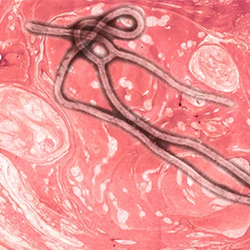
Ebola most commonly affects humans and nonhuman primates. Four orthoebolaviruses cause illness in people, presenting as clinically similar disease:
- Ebola virus (species O. zairense) causes Ebola virus disease.
- Sudan virus (species O. sudanense) causes SVD.
- Taï Forest virus (species O. taiense) causes Taï Forest virus disease.
- Bundibugyo virus (species O. bundibugyoense) causes Bundibugyo virus disease.
A person infected with Ebola disease is not contagious until symptoms appear, including fever, headache, muscle and joint pain, fatigue, loss of appetite, gastrointestinal symptoms, and unexplained bleeding. Ebola disease is spread through direct contact with the body fluids of a person who is sick with or has died from Ebola disease. Ebola disease is also spread by infected animals, or through direct contact with objects such as needles that are contaminated with the virus. Ebola disease is not spread through airborne transmission.
There is no FDA-licensed vaccine to protect against Sudan virus infection. The Ebola vaccine licensed in the United States (Ervebo, Merck) is indicated for preventing disease due to Ebola virus (species O. zairense) only, and based on studies in animals, is not expected to protect against SVD or other orthoebolaviruses. There is no FDA-approved treatment for SVD, but there are therapies in human clinical trials that are highly effective in animal models.
In the absence of early diagnosis and appropriate supportive care, Ebola disease has a high mortality rate. With intense supportive care and fluid replacement, mortality rates may be lowered. Previous outbreaks of SVD have had a mortality rate of approximately 50%.
The CDC has developed guidance for U.S.-based nongovernmental organizations and medical centers with staff working in the affected areas: Recommendations for Organizations Sending U.S.-based Personnel to Areas with VHF Outbreaks.
Contact your state, tribal, local or territorial health department immediately (via 24-hour Epi-on-Call contact list) if SVD is suspected, and follow jurisdictional protocols for patient assessment. If a diagnosis of SVD is considered, health departments will work with the CDC and clinical team to coordinate care and testing for the patient and ensure appropriate precautions are taken to help prevent potential spread.
Counsel patients with planned travel to an SVD outbreak–affected area about ways to prevent exposure during their travel.
Contact the CDC’s Viral Special Pathogens Branch (VSPB) 24/7 for consultations about SVD or other viral hemorrhagic fevers (VHFs). Call the CDC’s Emergency Operations Center at (770) 488-7100 and request VSPB’s on-call epidemiologist. For nonemergency inquiries, email spather@cdc.gov.
For suspect cases, request testing for SVD and other VHFs from the CDC (Atlanta) or the Laboratory Response Network (LRN). To date, 38 geographically diverse LRN laboratories and 13 Regional Emerging Special Pathogen Treatment Centers can test using the Biofire FilmArray NGDS Warrior Panel or Global Fever Special Pathogens Panel, with several more LRN laboratories expected to receive testing kits soon.
The Biofire Warrior Panel and Global Fever Special Pathogens Panel can detect orthomarburgviruses (Marburg and Ravn viruses) and orthoebolaviruses (Ebola, SVD, Taï Forest, Bundibugyo, and Reston viruses) in addition to other high-consequence pathogens.
Per the manufacturer’s recommendations, results from these test kits are presumptive, and require confirmatory testing, which can be performed at the CDC.