By Ethan Covey
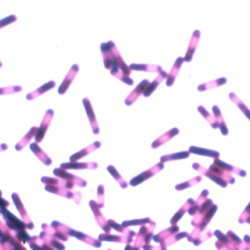
A study of data from Maryland found that Clostridioides difficile infection (CDI) case counts fell during the COVID-19 pandemic.
The study, which was presented at IDWeek 2023, held in Boston (poster 694), aimed to quantify the impact of COVID-19 on three classes of CDI cases: healthcare facility onset (HCFO), community onset-healthcare facility associated (CO-HCFA) and community associated (CA).
Population-based surveillance data for Maryland, collected through the Emerging Infections Program’s CDI Healthcare-Associated Infections Community Interface, were used to compare case details for pre-pandemic (2018-2019) and interpandemic (2020-2021) periods.
Across the state, 3,822 CDI cases were identified from 2018 through 2021. These included 1,142 HCFO, 771 CO-HCFA and 1,898 CA. During the pre-pandemic period, a total of 2,199 cases were identified, compared with 1,612 during the interpandemic period.
The decline began with a sharp drop during March 2020, and continued throughout the pandemic.
“This could be due to many reasons,” explained Kaytlynn Marceaux-Galli, MPH, an epidemiologist for the Maryland Department of Health in the Infectious Disease Epidemiology and Outbreak Response Bureau. “It could be that people didn’t seek out healthcare for testing not related to COVID; it could be increased awareness around handwashing. Either way we saw a huge dip in expected cases that first month of the pandemic.”
The researchers were interested in determining where, specifically, the decline in cases was centered.
“We wanted to know if there were certain cases that we saw less of—are we seeing fewer long-term care facility hospitalizations or community-associated cases?” Ms. Marceaux-Galli said.
Analysis revealed a few key findings:
- Interpandemic cases were 24% less likely to be CA and 31% more likely to be CO-HCFA than pre-pandemic cases; and although cases were 13% more likely to be classified HCFO, this increase was not significant between periods.
- Additionally, HCFO-long-term care facility cases were 26% less likely interpandemic than HCFO-hospital cases, and all-cause hospital admission for CDI was 27% less likely during the interpandemic period.
- CDI case counts increased for Black/African American individuals, and decreased for all other races, highlighting health equity concerns, according to the epidemiologists.
“Further investigation may determine whether changes in healthcare-seeking behavior, changes in infection prevention methods in long-term care facilities, local COVID-19 restrictions or other factors may have impacted CDI rates,” Ms. Marceaux-Galli concluded.
Ms. Marceaux-Galli reported no relevant financial disclosures.