By IDSE News Staff
People with HIV whose disease is not well controlled appear to be at greater risk for severe COVID-19 breakthrough infection after vaccination, according to a study led by researchers at the Johns Hopkins Bloomberg School of Public Health.

These findings suggest that this group should be considered for additional vaccine doses and other risk reduction measures.
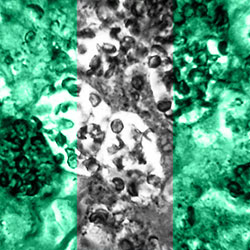
For the study, researchers analyzed data from the electronic health records of people with and without HIV. Of these, 3,649 people had breakthrough COVID-19 infection in the second half of 2021. Although vaccinations effectively reduce the risk for severe COVID-19 illness in both groups, people with HIV who had CD4 counts lower than 350 cells/mm3 of blood were 59% more likely to have severe breakthrough infections compared with those without HIV (JAMA Netw Open 2022;5[10]:e2236397).
The new study made use of the CIVET (Corona-Infectious-Virus Epidemiology Team)-II cohort, which included patients from the health systems of Kaiser Permanente Mid-Atlantic States, Kaiser Permanente Northern California, the Veterans Health Administration and the University of North Carolina. The initial study population included 33,029 people with HIV and 80,965 people without HIV who were fully vaccinated against COVID-19 during the period of December 2020 through June 2021. The two groups were matched by demographic factors such as age and sex, and by date of vaccination.
In the CIVET cohort, there were 3,649 cases of post-vaccination COVID-19 breakthrough infection (most were mild) in the two groups combined. In a companion study published in June, study senior author Keri Althoff, PhD, MPH, an associate professor in the Department of Epidemiology at the Bloomberg School, in Baltimore, and colleagues showed that these breakthrough infections happened at a higher rate in the HIV group, suggesting a 28% greater risk, compared with the non-HIV group. However, the level of absolute risk was low, at just 4.4% for the HIV group versus 3.8% for the non-HIV group.
In the new study, the researchers looked at the 249 cases of breakthrough infection that were classified as severe because they required hospitalization within 28 days of a COVID-19 diagnosis. They found that, while the risk for severe illness in the first 28 days was low and comparable between people with HIV (7.3%) and without HIV (6.7%), more immunocompromised people with HIV whose CD4 counts were lower than 350 cells/mm3 had a 59% higher risk than people without HIV.
Among people with severe breakthrough infections, 9.6% were mechanically ventilated (10.% in people with HIV and 9.4% in people without HIV) and 8% died during or within 30 days of hospitalization (7.5% in people with HIV and 8.2% in those without HIV) with no difference by HIV status.
“Clinicians who care for people with HIV with moderately low CD4 counts, that is with CD4 counts less than 350 350 cells/mm3, should encourage them to take additional precautions to prevent severe breakthrough COVID-19 illness,” Dr. Althoff added.
Currently, the CDC recommends people who are moderately or severely immunocompromised take additional precautions to protect themselves from COVID-19, including additional doses of vaccine.
The CDC recommends additional vaccine dosing and regular vaccine boosters for people who are moderately or severely immunocompromised. Although people do not need to prove their immunocompromised status to obtain extra vaccinations per the CDC’s guidelines, this category includes people with advanced or untreated HIV infection, defined as a CD4 T-cell count below 200 cells/mcL and an unsuppressed HIV viral load.
“People with HIV and CD4 counts between 200 and 350 cells/mm3 are not included in the current CDC recommendations,” Dr. Althoff said. “Our findings suggest people with HIV who have CD4 counts less than 350 cells/mm3 should be considered moderately or severely immunocompromised by the CDC, and encouraged to take additional precautions to protect themselves from severe COVID-19.”
Among vaccinated people with HIV, being older, being female or having a cancer diagnosis also was associated with a greater risk for hospitalization, whereas having had COVID-19 was associated with a lower risk.
The findings, according to Dr. Althoff, suggest that the CDC should consider broadening its recommendations for extra vaccine dosing to include people with HIV whose CD4 counts are below 350 cells/mm3.
The study was funded as a supplement to the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD, U01AI069918) from the National Institute of Allergy and Infectious Diseases.