Data from a pooled analysis of two trials found that one dose of rezafungin (RZF; Rezzayo, Melinta) demonstrated good safety and efficacy compared with caspofungin (CSF) to treat patients with candidemia or invasive candidiasis (CIC).
A negative blood culture result after treatment with RZF was also evident sooner compared with CSF, according to data that were presented at IDWeek 2024, in Los Angeles (poster P-1034).
The researchers analyzed the results of two clinical trials, phase 2 STRIVE and phase 3 ReSTORE, to compare a once-weekly oral dose of RZF with a once-daily infusion treatment with CSF for CIC, potentially fatal fungal infections. For this analysis, safety was measured in 151 people and efficacy in 139 people who received RZF; safety was measured in 166 people and efficacy in 132 people who received CSF.
Both drugs are in the class of echinocandins, a relatively new category used to treat fungal infections, said Luis Ostrosky-Zeichner, MD, FIDSA, the lead author of the poster, and a professor and the chief of the Division of Infectious Diseases at McGovern Medical School at UTHealth Houston.
The FDA approved RZF in 2023 based on the STRIVE and ReSTORE trials. Rates of cure and mycological eradication at day 14 and all-cause mortality at day 30 were comparable between the two treatment groups in both studies. STRIVE and ReSTORE were randomized, double-blind trials. Patients 18 years of age and older with CIC received once-weekly IV RZF (400 mg on week 1, then 200 mg weekly) or once-daily IV CSF (70 mg loading, then 50 mg daily) for 28 days, with 139 patients on RZF and 132 on CSF. The end points of the trial were all-cause mortality, mycological response and time to first negative blood culture at days 7, 14 and 30.
The goal of the study was to explore the potential benefit of just one dose of RZF for CIC, instead of two doses.
The mycological response was better in the RZF patients at all points: 99 versus 84 on day 7; 100 versus 88 on day 14; and 92 versus 77 on day 30.
However, more people died in the RZF group than the CSF group: 53 versus 48.
“The poster actually is about trying to see if we can push the envelope a little bit more,” Dr. Ostrosky-Zeichner said. “The current standard of care is to treat this infection for 14 days, and in this poster we explore whether the results at one week of treatment are similar to those at the end of the two weeks.”
Dr. Ostrosky-Zeichner said as far as the researchers could assess, “most of the outcomes happened within the first week, including negative blood cultures, … and do not change dramatically [at] week 2.”
He wanted to lay “the path” to see whether shorter durations of therapy were possible and appropriate for these patients.
“Patients want to be at home rather than in the hospital,” Dr. Ostrosky-Zeichner said, “and if they can be at home without any IVs, that’s even better. So our idea was whether we could explore the possibility that for uncomplicated cases of this type of infection, in the future, we could just give a single dose and then the patient is finished with the treatment.”
What was exciting for his research team, according to Dr. Ostrosky-Zeichner, was not only patient convenience but reduction of hospital stay and hospital-related complications, including the potential for other infections. “Completing therapy with a single dose for uncomplicated CIC could speed up hospital discharge and improve all sorts of economic metrics, for the patient as well as the hospital,” Dr. Ostrosky-Zeichner said.
It’s also important to emphasize that RZF seemed to clear the blood culture faster than the standard therapy, Dr. Ostrosky-Zeichner noted.
The next stage of the team’s research is to initiate a trial that would randomize patients to the standard therapy duration versus a short course to see whether they can confirm the findings of the poster, according to Dr. Ostrosky-Zeichner.
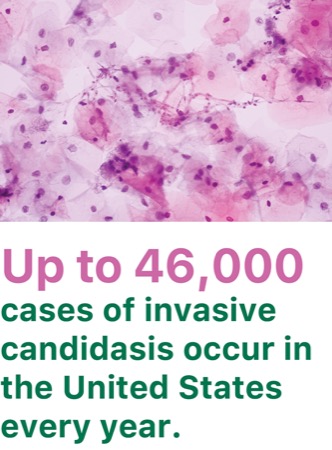
Yohei Doi, MD, PhD, a professor of medicine and the director of the Center for Innovative Antimicrobial Therapy at the University of Pittsburgh Medical Center, said there are many issues with CIC that make it critical for improved treatment including:
- a high mortality rate of 30% or higher, even with appropriate treatment; and
- the need for four weeks of daily IV treatment, which is inconvenient and expensive.
CIC used to be fairly sensitive to antifungal drugs, but more recently doctors in hospitals are seeing different species of Candida, which are often resistant to the drugs available, making new approaches to treating and combating the infection that much more crucial, said Dr. Doi, who was not involved with the research.
Although no new data were presented because the team analyzed the trials used to support the 2023 FDA drug approval, according to Dr. Doi, what is important here is that for antifungal drugs, “we usually look at outcomes data at one month, and here the team looked at data at one week to see efficacy.”
And what they found is that patients did as well with a conventional comparison drug at week 1 in terms of clinical improvement and time to achieving negative blood cultures—the data points physicians look at to see how their patients are doing, according to Dr. Doi.
“The poster by Dr. Ostrosky’s team won’t change what we do immediately, of course,” Dr. Doi said, “but I do think it informs what kind of studies that the team or other investigators may envision in terms of optimizing the use of this new antifungal agent, rezafungin, safely.”
Dr. Ostrosky-Zeichner reported that he is an advisor for/consultant to Cidara, Enanta, Eurofins Viracor, F2G, Gilead, GSK, Melinta, Octapharma and Pfizer; and receives grant/research support from Pfizer, Pulmocide and Scynexis. Dr. Doi reported no relevant financial disclosures.
This article is from the February 2025 print issue.