Invasive mycoses are a leading cause of mortality among patients with advanced HIV disease, often resulting in death even among patients who receive antifungal therapy.
A pair of studies presented at CROI 2024, held in Denver, sought to examine the burden of mycoses and the importance of testing for mycoses among people with advanced HIV.
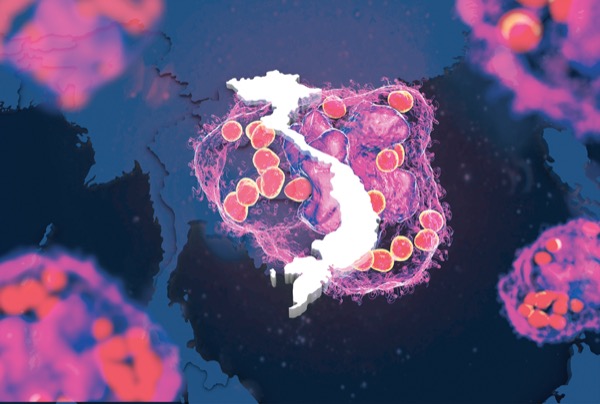
The researchers sought to study rates of histoplasmosis among people with advanced HIV in Vietnam (poster 895).
“The study has a focus on histoplasmosis and is part of a larger project to screen for invasive fungal infections in patients with advanced HIV disease,” said Hao Nguy?n, MD, of the Oxford University Clinical Research Unit, in Hanoi, and the lead author of the poster. “The project explores the impact of adding fungal antigen tests and fungal blood culture in addition to the standard of care, which currently includes only standard cultures of clinical specimens requested by a treating doctor.”
Between February 2021 and November 2023, the researchers recruited 901 patients with a CD4 count less than 100 cells/mcL or with stage 3 or 4 HIV by World Health Organization criteria. The patients also were hospitalized for any symptoms.
Histoplasmosis testing was conducted using the IMMY Clarus Histoplasma GM enzyme immunoassay (HAg EIA). The test identified that 3% of patients hospitalized with advanced HIV in Vietnam had disseminated histoplasmosis. The HAg EIA was found to have excellent diagnostic performance, with a sensitivity of 100%, specificity of 99.2%, accuracy of 99.9%, positive predictive value of 79.4% and negative predictive value of 100%, according to the researchers.
Additionally, the team’s screening program identified talaromycosis (formerly known as penicilliosis) in 19.8% of patients and cryptococcosis in 4.7%.
Mortality was very high, even when appropriate therapy was initiated.
“One in five patients die despite antifungal therapy,” Dr. Hao told Infectious Disease Special Edition. “This is an important finding because without screening, 65 patients with these invasive fungal infections (25%) would have been missed, and these infections are uniformly fatal if not timely diagnosed and treated.”
The study also assisted in clarifying the risk for these mycoses in Southeast Asia.
“While talaromycosis and cryptococcosis are known to be highly endemic in Vietnam, little is known about the burden of histoplasmosis in Vietnam and Southeast Asia,” he said. “It was previously thought that histoplasmosis is endemic only in the central and southern United States and Latin America. Our study reveals a more widespread endemicity of histoplasmosis and highlights the importance of raising awareness of histoplasmosis and the need to screen for these invasive mycoses using antigen tests and fungal cultures in patients with advanced HIV disease in Southeast Asia.”
The researchers showed invasive mycoses accounted for 27.3% of inpatient, and 9.5% of outpatient, visits among people with advanced HIV disease in Vietnam (poster 890). When tuberculosis and non-TB mycobacteria are included, they account for just more than half (54.8%) of inpatient visits, and 17.6% of outpatients.
The findings stressed the need for increased awareness of, and screening for, these invasive mycoses.
“Given the high mortality of these fungal infections despite antifungal therapy, further research to determine whether screening for talaromycosis and histoplasmosis earlier, in asymptomatic patients with advanced HIV in clinic, will improve patient outcomes and reduce mortality,” said the senior authors Rogier van Doorn, MD, PhD, a clinical microbiologist at Nuffield Department of Medicine, at the University of Oxford, England, and Thuy Le, MD, PhD, an associate director of the Duke CFAR Clinical Core.
“In our study, nearly 30% of patients with histoplasmosis died despite screening and treatment. The true mortality is expected to be much higher outside of this research study as antigen testing and fungal culture are not being done. Future work focusing on increasing awareness of invasive fungal infections and advocacy for implementation of antigen testing and fungal culture is urgently needed.”
Both studies were the result of a collaboration among Duke University School of Medicine, Oxford University Clinical Research Unit in Vietnam and three large referral hospitals in Vietnam.
The National Institutes of Health provided funding for this research. The researchers reported no relevant financial disclosures
This article is from the June 2024 print issue.