A study focused on the distribution of mpox vaccines in Durham County, N.C., illustrates how persistent, targeted outreach efforts can address successfully issues caused by social determinants of health (SDOH) and social vulnerability, allowing for increased vaccine uptake among high-risk individuals.
These findings, the researchers of the study wrote, may help address underlying factors associated with vaccine reception, and assist with outreach to historically marginalized populations (J Racial Ethn Health Disparities 2024;11[6]:3768-3772. bit.ly/4gjqnLq-IDSE).
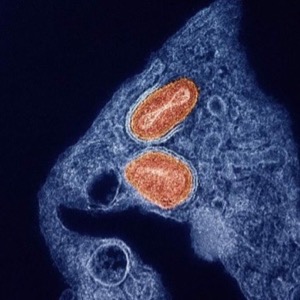
“We started offering free mpox vaccination at the Durham County Department of Public Health starting in the summer of 2022 during the height of the mpox clade IIb global outbreak,” Jeffrey D. Jenks, MD, an adjunct associate professor of medicine in the Division of Infectious Diseases at Duke University, in Durham, N.C., and senior researcher of the study, told Infectious Disease Special Edition. “At this time we also engaged in extensive outreach efforts to members of the community who were most at risk for mpox at that time.”
The outreach efforts included partnering with Duke Health to administer mpox vaccinations during Durham Pride in September 2022, collaborating with the LGBTQ Center of Durham, hosting webinars and communicating on social media.
“We feel that these outreach efforts, in addition to offering a convenient way to get the mpox vaccine free, allowed us to successfully reach individuals most at risk for mpox infection,” Dr. Jenks added. “This included individuals living in census tracts with high social vulnerability and groups who are historically undervaccinated, including Black or African American and Hispanic or Latino individuals.”
The analysis of the efforts’ effectiveness focused on data collected from Aug. 8, 2022, to Jan. 18, 2023. During this time, 2,113 doses of the Jynneos mpox vaccine (Bavarian Nordic) were administered in Durham County. Random forest regression and min-max scaling were used to predict mpox vaccinations in the county at the census tract level. Additionally, top SDOH and social vulnerability index (SVI) features and how they correlated with vaccination were assessed.
Men living with another male partner were most significantly associated with mpox vaccination over other groups. The SVI features most associated with receipt of the mpox vaccine were age 25 years and older without a high school diploma, noninstitutionalized people lacking healthcare, those 16 years of age and older who were unemployed, living 150% below the federal poverty level, and living in a household without a vehicle. Identifying as Black or African American, Hispanic and Latino, or otherwise non-white were also associated with receiving the mpox vaccine.
“This study reinforced the practice of collecting individual social determinants of health responses,” said Savannah Carrico, MPH, a public health epidemiologist with the Durham County Department of Public Health and first author of the study. “For example, individuals that came to the health department to receive their vaccine were given an additional questionnaire asking about HIV status, gender identity, address, race, etc.
“In the future at the health department, we’d like to implement this questionnaire for all emergent services so we can collect real-time and accurate data about the populations we are able to reach,” Ms. Carrico said.
Tom Carpino, MPH, the Gordis Teaching Fellow at Krieger School of Arts and Sciences and a PhD candidate in infectious disease epidemiology at the Johns Hopkins Bloomberg School of Public Health, in Baltimore, told Infectious Disease Special Edition that “this article has surprising findings and suggests that with concerted and targeted outreach and sufficient public health infrastructure and prioritization, vaccine access for key populations is possible, even among people who are uninsured.
“As [the] number of vaccine doses received is very important for prevention, I am curious to see an analysis on predictors of receiving two or more mpox vaccine doses,” Mr. Carpino, who was not involved with the research, added.
Dr. Jenks pointed out that additional work may help build upon the study, since this project only looked at vaccination against one vaccine-preventable disease in one setting, and looked at social vulnerability and some key SDOH from the census tract level only.
“Future research should investigate how social vulnerability relates to vaccine reception for other vaccine-preventable diseases, particularly using individual-level demographic and social determinants of health data, from which stronger conclusions can be drawn,” he said.
Overall, however, he noted that the findings provide strong support for efforts aimed at targeting high-risk individuals.
“Our findings show that populations who are socially vulnerable can successfully be reached to receive vaccines for vaccine-preventable diseases with aggressive outreach efforts and partnership with trusted individuals and organizations in those communities,” Dr. Jenks said.
Dr. Jenks reported research funding from Astellas, F2G and Pfizer—all unrelated to this work. Mr. Carpino and Ms. Carrico reported no relevant financial disclosures.
This article is from the February 2025 print issue.