Intensive care units are particularly challenging environments for pursuing antimicrobial stewardship (AMS) in a hospital.
“There is high acuity and patient complexity in the ICU; these patients are very sick,” said Rebekah Moehring, MD, MPH, an associate professor of medicine in the Division of Infectious Diseases at Duke University School of Medicine, in Durham, N.C. “Many of them have fever and white cell elevation, sometimes due to infection and sometimes due to other causes, and it can be difficult to tease out disease states clinically,” she said.
“They also have a high prevalence of antimicrobial exposure and a high risk for acquiring multidrug-resistant organisms and/or hospital-acquired infections,” Dr. Moehring added.
Unique Workflow, Culture
Each ICU also has a unique workflow and culture, particularly in more specialized units such as neuro ICUs. “Not only are they unique in the types of patients they care for, but they often have their own hierarchy and style of communication,” Dr. Moehring said. “Your antimicrobial stewardship strategy in ICUs will need to differ based on that underlying model, their existing practice and their patient population.”
In a study published in Clinical Infectious Diseases, part of a relatively small body of evidence studying the effects of stewardship in the ICU setting, Dr. Moehring and colleagues found that changes in antibiotic use (AU) after implementation of dedicated weekly antibiotic stewardship rounds varied widely by unit. For example, changes in AU were the largest in the neuro ICU (–28%) and smallest in the cardiothoracic ICU (–2%) (Clin Infect Dis 2022;74[11]:1986-1992).
“Antibiotic stewardship ICU rounding is a high-resource intervention, but effective in reducing AU and building qualitative knowledge and relationships between ICU and [antibiotic stewardship] teams,” they wrote.
As a result of their findings, the Duke ID team adjusted its AMS strategy for the ICUs, increasing the frequency of rounds in ICUs where the house staff do not routinely get significant antibiotic input from attendings and where the culture is more receptive to AMS input. They also changed the roles for stewardship pharmacists and physicians. Physicians now focus on chart review for diagnostic opportunities and antibiotic-use rationale in the ICU with support from pharmacists for dosing and duration, while stewardship focuses on chart review outside of the ICU with support from physicians for diagnostic challenges.
Who Makes the Decisions?
“To be successful in antimicrobial stewardship in any ICU, you first need to identify their practice model,” Dr. Moehring said. “Who makes the decisions about antibiotics in this ICU? What role do they play in the team dynamics and hierarchy? What is the workflow and timing of antibiotic decision making, including timing of rounds? Decide who could be your key partners and allies, and identify who may be your challengers.”
ICU clinicians are apprehensive about adjusting and de-escalating antibiotics in critically ill patients, Robert Granett, PharmD, BCPS, a clinical pharmacy specialist at Covenant HealthCare, in Saginaw, Mich., noted in a separate interview. Dr. Granett has published on the role of pharmacists in AMS in the ICU setting. “One of your biggest challenges will be balancing the concern over missing a bacterium with the risk for overtreating. Rapport with providers is essential, and you really must show your worth.”
Check Priorities With Team
The next step: Frame a problem of interest. “Have at least a couple of ideas in mind. What you think is high priority may not match what the critical care team thinks is important,” Dr. Moehring said.
“Take a walk in critical care’s shoes. Why should they make this issue a high priority? Identify data or perspectives that you may want to bring to them to make sure that they’re engaged and on board. Consider using safety events; patient-level stories are very compelling,” she said.
Low-hanging fruits for ICU intervention include bug–drug mismatches and renal changes, Dr. Granett said. “We use the integrated Epic application Bugsy, which helps us pick those out,” he said. “The biggest challenges include dealing with patients whose condition is so delicate that a bacterium that is missed could lead to worsening sepsis and death. You must balance that with all the collateral damage that goes along with inappropriate antibiotic use, including cardiac toxicity, nephrotoxicity and creating superbugs.”
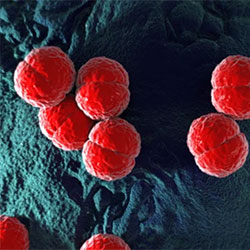
Rapid diagnostic testing is particularly useful in these situations, he said, describing the recent case of a patient in the ICU who was being evaluated for positive blood cultures for gram-positive bacteria. “[ID clinicians] wanted to add vancomycin, but the patient was already in the early stage of acute kidney injury,” he said. “I reached out to microbiology, and we had only five minutes remaining for results on the about 45-minute testing period. Lo and behold, it was MSSA [methicillin-susceptible Staphylococcus aureus], not MRSA [methicillin-resistant S. aureus], so we avoided vancomycin and further toxicity.”
Keep a Flexible Time Line
The time line of an AMS intervention in the ICU needs to be variable and adaptable. “You may want to consider a small pilot study to work through process issues and estimate sample size impact,” Dr. Moehring said. “Start with your favorite ICU instead of launching simultaneously in five ICUs like we did. That will allow you to develop more information about how much work it is and where are the areas of miscommunication that you need to think through more carefully.”
The next step is to determine how to assess the effect of a given ICU stewardship strategy. Both primary and secondary outcomes, including balancing metrics, are needed, Dr. Moehring stressed. “You want to be sure to include the things that you don’t intend to move the data on with your strategy, and you don’t want that strategy to result in [negative] events or deaths,” she said. “So you need to be able to assure your critical care partners that [the measures] are safe for patients.”
Don’t get discouraged if early ICU stewardship efforts do not meet with success. “Your first attempts are not likely going to be winners,” Dr. Moehring said. “You must be constantly reassessing and reframing the problem. Antimicrobial stewardship strategies in the ICU must be adaptive.”
The sources reported no relevant financial disclosures. Portions of this article were based on presentations at the 2023 MAD-ID (Making a Difference in Infectious Diseases) annual conference, in Orlando, Fla.
This article is from the April 2024 print issue.