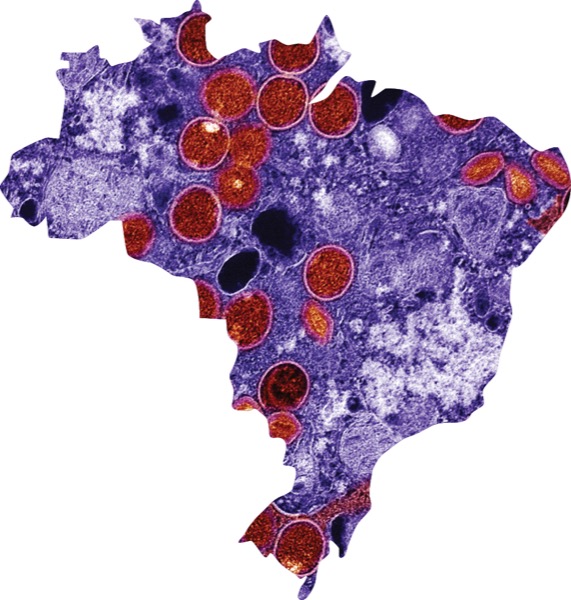
Mpox continues to be an international problem, reminded Mayara Secco Torres da Silva, MD, who presented data at CROI 2024, about a recent mpox outbreak in Brazil (abstract 198).
As of Jan. 28, 2024, Brazil reported around 11,000 cases of confirmed mpox, 16 deaths and another 349 probable cases.
The World Health Organization declared an mpox public health emergency on July 23, 2022, after a large, international outbreak primarily among men who have sex with men (MSM). Cases finally began to decline after several actions, including vaccination campaigns, and the WHO ended the emergency in May 2023, because of the declines.
The only problem is that mpox hasn’t gone away, Dr. da Silva said. “Our results emphasize the crucial need to enhance continued surveillance strategies to promptly detect emergent STIs [sexually transmitted infections] within the context of HIV care and prevention services. As community transmission advances, people living with HIV who are not engaged in HIV care—both late presenters and those who are lost to follow-up—might be increasingly more affected and vulnerable to severe courses of mpox,” she said.
Brazil’s Experience
Rio de Janeiro was one of the epicenters of the mpox outbreak in Brazil, according to Dr. da Silva. The Evandro Chagas National Institute of Infectious Diseases at Cruz, a major infectious diseases referral center in Rio de Janeiro, established the INI-Fiocruz mpox cohort to follow the cases. “This ongoing prospective cohort has enrolled individuals with suspected mpox since the first outbreak in June 2022,” she said.
Through this surveillance cohort, the researchers found evidence of an emerging second outbreak of mpox in Rio de Janeiro.
“Since late September 2023, we have observed a steady and progressive increase in mpox diagnosis with 117 persons with confirmed mpox until January 2024,” Dr. da Silva said.
They compared the characteristics of people with confirmed mpox in the second outbreak with those in the first and saw similarities, but also notable differences.
“So far, individuals self-identifying as Black or Pardo [an ethnic and skin color category used by the Brazilian Institute of Geography and Statistics] and from lower educational backgrounds have been disproportionally affected throughout both outbreaks,” she said (Black/Pardo: 234 [60.1%] vs. 79 [68.7%]; primary school: 232 [58.1%] vs. 70 [60.3%]; secondary school: 32 [8%] vs. six [5.2%]; post-secondary school: 135 [33.9%] vs. 40 [34.5%]).
The second mpox outbreak affected mostly cisgender men between 30 and 39 years old, and there were fewer reports among cis- and transgender women compared with the first outbreak. However, most cases continue to occur among MSM, especially those reporting more sex partners and anal sex in the 30 days prior to symptom onset.
The researchers also saw a higher percentage of people with HIV or who were taking pre-exposure prophylaxis in the second outbreak than the first, as well as a higher prevalence of concomitant bacterial STIs, especially syphilis and hepatitis C virus, according to Dr. da Silva.
“Altogether, among the 306 participants diagnosed with mpox and also living with HIV during both outbreaks, about 15% had HIV viral loads higher than 200 cell counts/mL, whereas 13% had CD4 cell counts below 350 cells/mm3, evidence of an advanced degree of HIV-related immunosuppression across outbreaks,” Dr. da Silva said.
“Higher rates of concomitant opportunistic infections have been reported in the current outbreak, and mpox-associated immune reconstitution inflammatory syndrome was suspected in about 4% of cases.
“This highlights the importance of further understanding the synergy between mpox and HIV coinfection,” she said.
Because the new cases followed a period without signs of sustained transmission, Dr. da Silva said clinicians may have had a lower threshold of clinical suspicion for mpox.
The American Experience
Continuing mpox is also happening in the United States, including New York City, where Mary Foote, MD, MPH, is the medical director of the NYC Department of Health and Mental Hygiene.
“We have definitely seen an increase in cases over the past few months in New York, but the overall numbers are still low,” she told Infectious Disease Special Edition. “We think there are a lot of cases being missed due to providers not considering it in the differential and not testing since most of our cases are locally acquired, which implies consistent ongoing community transmission.”
Since Jan. 1, 100 people in the city have tested positive for mpox—37 between Feb. 11 and March 9.
Although greatly diminished, the United States is still seeing mpox cases, confirmed CDC Senior Public Affairs Officer Tom Skinner, of the National Center for Emerging Zoonotic Infectious Diseases. As of March 26, the CDC has reported 511 cases of mpox in the United States and its territories this year (wonder.cdc.gov/nndss/static/2024/11/2024-11-table968.html).
Because of ongoing transmission, “we are gearing up for a busier summer this year compared with last,” Dr. Foote said. “There are also some big European festivals coming up in April and May that will likely have some impact here with imported cases—like we saw in 2022—so, we are advising provider vigilance and to have a low threshold to test and to also be proactive in ensuring patients at risk receive the full two-dose vaccination series.”
The city is planning public health campaigns geared toward providers and the community over the next few months. However, they don’t expect the public health emergency seen during the first outbreak because so many of those at high risk in the United States were vaccinated or previously infected, so disease should be milder for many this year. However, Dr. Foote reminded, mpox can be fatal, especially in people living with advanced HIV, so “extra effort should be made to do proactive outreach to these patients to ensure they are protected and seek care if they develop symptoms.”
This can be a fatal disease, especially in people living with advanced HIV, so extra effort should be made to do proactive outreach to these patients to ensure they are protected and know to seek care if they develop symptoms.
“Vaccination is still being encouraged and recommended for those at highest risk for mpox in the United States,” Mr. Skinner said. This group includes MSM, transgender, gender nonbinary or gender diverse people, as well as anyone who has sexual or intimate contact with someone who might have mpox, regardless of their sexual or gender identity. (For more, see www.cdc.gov/poxvirus/mpox/vaccines/index.html.)
“Two doses provide the best protection. Get dose 1, wait four weeks, and then get dose 2,” Mr. Skinner said. It takes about two weeks after the second dose to build up the maximum immunities, he added. (To find a vaccination location, see www.cdc.gov/poxvirus/mpox/vaccines/vaccine-recommendations.html.) The CDC recommends that people get the second dose even if it has been more than four weeks after the first dose.
Dr. da Silva said Brazil still has not implemented a national mpox vaccination campaign for the LGBTQIA+ community, which is sorely needed in her country.
She called for “consistent efforts to control mpox, emphasizing the need for a more equitable distribution of health technologies across the globe and for tackling structural determinants that impact the HIV continuum of care outcomes.”
The sources reported no relevant financial disclosures.
This article is from the April 2024 print issue.